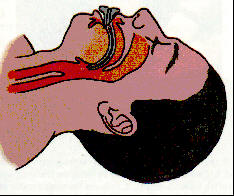
An oropharyngeal (OPA) airway is used to help establish a
patients airway when a is not present. OPAís come in many sizes. To ensure proper size the
rescuer should measure by placing one end of the device on the corner of the
and the other end to the earlobe. To insert the OPA, hold the device
at its flange end and insert it into the mouth with the tip pointing toward
the roof of the patientís mouth. Once the distal end of the OPA reaches the
posterior wall of the pharynx, rotate the OPA 180 degrees so that it is
positioned over the tongue. The flange should rest on the
when properly inserted. Use of the OPA does not eliminate the need
for maintaining proper head position.
 It is
also acceptable to rotate the device at 90 degrees.
It is
also acceptable to rotate the device at 90 degrees.
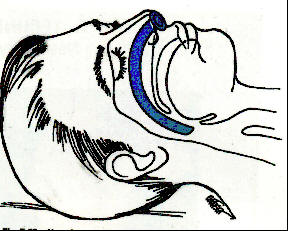
Nasopharyngeal Airway (NPA)
The NPA is used when the oral pharynx is not accessible or the patient has a gag reflex. The device is contraindicated in patients with and used with caution if are present. To ensure proper size the rescuer should measure from the corner of the to the earlobe. Lubricate the device prior to placement with a water based substance. When inserting the NPA in an emergency on should pick the largest and straightest nostril. Place the bevel of the NPA to the nasal septum. Hold the device like you would a pencil and slowly insert the NPA into the patientís nostril until the flange is flush with the nostril. Do not force the device. Use of the OPA does not eliminate the need for maintaining proper head position.
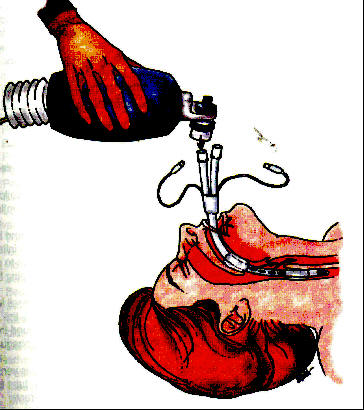
Mouth-to-Mask and Bag-Valve-Mask
Mouth-to-mask breathing is the preferred method of ventilating a nonbreathing patient. It is a simple one person device, and because of the two-handed mask seal it provides excellent ventilatory volumes. The device when not connected to supplemental oxygen will deliver % oxygen to the patient. When attached to >10 LMP of supplemental oxygen the device delivers approximately % oxygen.

The bag-valve-mask (BVM) consists of a -way valve, -inflating bag, reservoir, and a mask. The device delivers % oxygen concentration with room air and once connected to high flow
supplemental oxygen it can deliver up to 80 to % oxygen concentration. The BVM technique commonly creates a poor
seal around the patientís mouth and is designed for two trained rescuers to
use. The BVM typically delivers volume than mouth-to-mask technique. When using a BVM during a
cardiac arrest the rescuer needs to be aware of the pop-off valve status
because greater ventilatory pressure is usually required. This device is most
effective when the patient is intubated and the BVM is attached to an
endotracheal tube (ETT) because the trachea is then isolated.
Tidal Volumes and Inspiratory Times
If supplemental oxygen is not available, tidal volumes and inspiratory times should be approximately mL/kg (800mL) and delivered over 1 second which is sufficient to make the chest rise.
If supplemental oxygen is available, lower tidal volumes are recommended. A tidal volume of approximately 6 to 7mL/kg (500mL) is given over 1 second. The delivery of lower tidal volumes should reduce the risk of gastric inflation and its consequences.
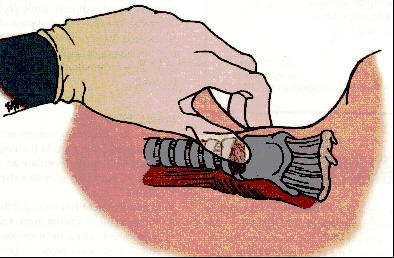
Sellickís Maneuver (Cricoid Pressure)
Sellickís maneuver reduces gastric inflation during ventilatory efforts. By placing downward pressure on the cartilage the diameter of the esophagus is decreased therefore restricting the flow of air into the stomach.
Suction
If a patientís airway is compromised by fluids, turn the victim head to one side and remove large particles. Once suction is available the remaining fluids and fine particles should be removed. For oral suctioning the pressure should be set at approximately mmHg and suction limited to seconds. For tracheal suctioning the pressure should be around to 120mmHg and suction time limited to seconds. Only suction on the way out and always measure for proper advancement depth of the suction catheters.
Advanced Airway Management
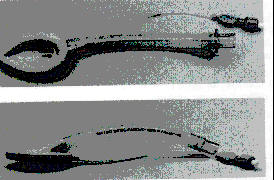
Esophageal-Tracheal Combitube (ETC)
The ETC allows ventilation of the lungs and reduces the risk of aspiration of gastric contents. The device is inserted to ventilate the trachea, regardless of esophageal or tracheal placement. If the tube is placed in the trachea the distal cuff is inflated with up to 15 to 20mL of air. If the ETC was placed in the esophagus inflate the proximal cuff with up to 100mL of air to seal the pharynx and inflate the distal cuff with up to 15 to 20mL of air to seal the esophagus. Air will then be directed to the trachea. Contraindications: gag reflex present, suspected disease, ingestion of substance and patients less than feet tall (37F or 39F size). 41F size is for 5 feet to 6 foot 7 inch patients. 37/39F is for patients that are 4 feet to 5 feet. All patients must be over years of age to use. Do not use if caustic ingestion or esophageal trauma is present.
Pharyngotracheal Lumen Airway (PTL)
A duel-lumen tube that allows either tracheal or esophageal placement. The PTL is blindly inserted just like the ETC. Consists of two parallel tubes of equal length and two balloon cuffs that inflate simultaneously when air is blown into the inflation port with a bag-valve device. When inflated one cuff closes the oropharynx and the other cuff secures the esophagus or trachea depending on distal placement. Contraindications: gag reflex present, patients less than 5 feet tall, patients less than 14 years old, suspected esophageal disease, and ingestion of caustic substance.
King SupraGlottic LTS-D Airway
King
Systems' KING LTģ airways are the industry's first supraglottic airway devices
designed for positive pressure ventilation over 30 cm H2O
as well as for spontaneous breathing. Both the reusable KING LT and
disposable KING LT-Dô and KING LTS-Dô are easy to insert and cause minimal
airway trauma. Their soft, inflatable cuffs provide stability with a superior
airway seal and they are 100% latex free. The KING LTS-D offers the unique
ability to pass a gastric tube through a second channel of the airway into the
stomach. The EMS KING LT-D and KING LTS-D are packaged as kits and are sold
exclusively by Tri-anim.
King Systems also offers a versatile Cuff Pressure Gauge that measures both
endotracheal tube and supraglottic airway fill pressures.
Size: #3, #4, and #5. If using a size # the patient should be 4 feet to 5 feet. Size # is 5 feet to 6 feet and size #5 is 6 feet to 7 feet.

Laryngeal Mask Airway (LMA)
The LMA may be used as an alternative to either the endotracheal tube (ETT) or the face mask with either or positive-pressure ventilation. The LMA may be used as the airway, as a channel for an ETT, or as an option in the management of a difficult airway when intubation is unsuccessful. The device consists of a tube that is fused to a elliptical, spoon-shaped mask at a 30-degree angle. The LMA comes typically in sizes, number 1 through 5. Size fits a 30 to 50kg pt and size 5 is for 70kg and greater. When inserted, the tube protrudes from the patientís mouth and is connected to a ventilation device. The mask is advanced until resistance is felt. Then the mask is inflated, it provides a low-pressure seal around the laryngeal inlet. When the LMA is properly placed, the black line on the tube should rest in the midline against the patientís upper lip. The LMA is contraindicated if a risk of aspiration exists. Some physicians prefer to rotate the LMA 90 degrees during insertion but the standard way is directly in. Also KY gel should be added the the distal posterior portion of the LMA. Do not use if caustic ingestion or esophageal trauma is present.
Endotracheal Tube (ETT) Intubation
ETT intubation is the airway of choice for all critical patients who cannot protect their own airway. Tube advancement is directly into the trachea and a cuff is inflated with up to mL of air to secure the trachea. Advantages to ETT intubation are of the trachea, reduction in the risk of aspiration, eliminates the need to maintain a mask seal, direct route for tracheal suction and certain medications can be administered via the ETT. Disadvantages are that it takes more skill than other airway devices, ETT can be easily, and takes more equipment than other methods to secure an airway. It is also recommended to use a commercial grade tube tie device to secure the ETT.
Tube sizes: range from 2.5 mm to 9 mm. Size 7 to 8 for men and size to 7 for women. If patient is less than years of age it is not recommended to inflate the cuff.
Blades: (Wisconsin or straight) comes in 5 sizes. MacIntosh is a curved
blade and comes in 5 sizes.
Miller is placed on the epiglotis and lift. MacIntosh is placed in the
and lifted to raise the epiglottis.
Stylet provided shape and rigidity to the ETT while placing.
Prior to Advanced Airway Placement
Patients should be hyperventilated and well oxygenated for minutes at a rate of per minute before placement of an advance airway device. The attempt to establish the airway device should take no longer than seconds to complete. If the device cannot be established within 30 seconds the patient should be hyperventilated again for 2 minutes before the next attempt.
Airway Placement Confirmation
Whenever airway assistance is being provided the rescuer should ensure proper ventilation of the patient two ways: with confirmation techniques and confirmation techniques. Primary confirmation techniques include 5-point , bilateral chest expansion, and mask or tube condensation. In secondary confirmation techniques, detector devices are preferred for intubation confirmation in adult cardiac arrests; end-tidal detectors (capnography, capnometry, capnometer) are preferred in non-cardiac victims.